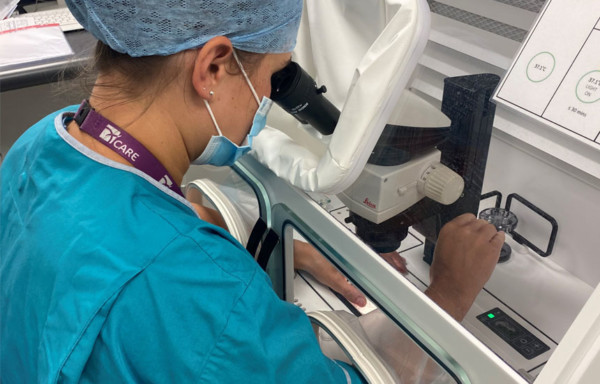
An interview with Dr. Amy Barrie, Laboratory Manager, Chester and Liverpool, CARE Fertility, UK and
Dr. Michael J. Tucker, Scientific Director, Shady Grove Fertility, USA
Advancements in IVF have brought greater efficiency and accessibility to those who seek to become parents, but fertility clinics today face many challenges to ensure the best fertility journey for every patient. We spoke with Dr. Barrie, CARE Fertility Laboratory Manager and Dr. Tucker, Shady Grove Fertility Scientific Director, who both have implemented the electronic witnessing system (EWS) RI Witness™ into their labs to discuss how digital and automated integration can support clinics and patients throughout the entire fertility journey and play a role in improving lab performance.
Dr. Amy Barrie is the Laboratory Manager and Human Fertilization and Embryology Authority (HFEA) Person Responsible at CARE Fertility Chester and CARE Fertility Liverpool. Dr. Barrie is a Consultant Clinical Scientist and a member of the Fellows of the Royal College of Pathologists.
Dr. Michael J. Tucker is the Scientific Director at Shady Grove Fertility since 1998. Dr. Tucker is certified as a High-complexity Clinical Laboratory Director (HCLD) in the United States and is a fellow of the Institute of Biology in the United Kingdom.
Shady Grove Fertility and CARE Fertility could both be described as high-volume clinics. What are some of the challenges that you face?
Dr. Barrie: CARE Fertility clinics have grown in number. With thirteen full labs in the UK and Ireland as well as eight satellite clinics, we are conducting around ten thousand treatment cycles every year. One thing we have started to see in recent years is that for patients, the journey and the outcome are intertwined. It is an emotional experience for patients, so they want to be more informed and feel empowered. Making the journey more transparent creates an opportunity to continue to build trust with our patients.
Dr. Tucker: In 2021 alone, Shady Grove Fertility (SGF) has grown from nine to eleven U.S.-based IVF laboratories, increasing our IVF cycles to almost 10,000 a year, including frozen embryo transfers. This growth comes at a pivotal time when SGF is also celebrating its 30th anniversary and the monumental milestone of 100,000 SGF babies born — an accomplishment that is a direct reflection of SGF’s focus on cutting-edge science, technology, and management. While we are proud of this growth, we are fully aware that this increase in volume can come with some risks.
I take my role as Scientific Director very seriously and see myself as a risk manager more than anything by ensuring chain of custody in three areas: the right embryo or gamete for the right patient, vitrification process, and bio cryopreservation. SGF has always had a strong focus on documenting the patient’s entire fertility journey. As SGF grows, we are continuously seeking opportunities to fortify our already strong chain of custody.
“Making the journey more transparent creates an opportunity to continue to build trust with our patients.” – Dr. Barrie
Manual double witnessing is essential yet can be a time-consuming protocol in clinics. Was that one of the reasons you chose an electronic witnessing system such as RI Witness?
Dr. Tucker: Yes, every step needs to be double witnessed by two embryologists, including documentation throughout the whole IVF process, which means enough staff must be scheduled. For any sized laboratory, an EWS is immediately appealing.
We are always open to new technologies that can improve the IVF process. The incubation process is a great example of how technology has minimized embryo stress. Today, an EWS can support quality control in fertility labs, such as helping to maintain consistent temperatures within culture media by shortening the time required for double witnessing.
Dr. Barrie: Manual double witnessing is an engrained part of an embryologist’s role in the lab. It is just built into our training that you need a witness. Today, even with an EWS, there are certain steps, entry and exit points and the mixing of gametes that still need to be manually witnessed. But to go from double witnessing every single IVF step to only these few points is a big improvement. We are very busy every day, with patients and in the lab, so timesaving is an integral part of a smooth-running clinic.

What are the benefits of RI Witness in your clinics?
Dr. Barrie: RI Witness is the sleekest system I have worked with. I cannot think of a better word to describe it. The RFID technology is intuitive, immediate and adjustable, so you can tailor it to your clinic, which is really good.
In our experience, the barcoding system was not immediate as sometimes the barcodes were hard to read. So, the RFID tags being more consistently readable was a happy surprise for the lab staff.
The best thing is that RI Witness is just happening, recording everything going on in the lab. And as well as not disrupting a second embryologist, now you do not have to wait with culture dishes out of the incubator, exposing the gametes and embryos to suboptimal conditions for a protracted length of time.
Dr. Tucker: As the largest fertility clinic group in North America, the benefits of RI Witness start with freeing up time. The ability not to have to need a second embryologist for each of the steps throughout the process. So for us, the clearest and immediate benefit was less pressure on our staff and a decrease in staffing demands.
As a quality management tool, RI Witness task logs are automatically updated. RI Witness has the ability to have a full task log to observe what is happening across any given lab during any given day. And a well-documented task log for each individual patient or couple certainly stands well in terms of inspection and enables us to make certain that our chain of custody integrity is fully intact.
IVF Witness System: RI WitnessTM ART Management System
Can you talk about the setup process?
Dr. Tucker: We began to consider the rollout of RI Witness across each of our labs in 2019. Currently, nine out of our eleven labs have adopted RI Witness, so it is relatively recent. Post setup, there are oversight and lab leadership meetings every four to six weeks to answer questions and concerns.
As a long-term investment, the adoption of the RI Witness system provides higher quality management and more transparency while working more efficiently. Together with the CooperSurgical team, we have worked through a tough 2020 and I am proud that we soon will have the full setup across our clinics.
Dr. Barrie: We made the decision around 2018 and then the implementation process of RI Witness has been happening over the last couple of years. By 2020, RI Witness was fully installed in all our clinics. We had regular meetings with CooperSurgical’s RI Witness Team every 2 weeks during setup and whether for 5 minutes or an hour, they were readily available to help.
Implementing RI Witness into a clinic system is a process that takes time. By putting in the work to get the system right, when it is up and running, it will certainly make any lab more efficient.
“As a long-term investment, the adoption of the RI Witness system provides higher quality management and more transparency while working more efficiently.” – Dr. Tucker
What excites you about the potential RI Witness has across all your clinics?
Dr. Barrie: We recently reached a milestone with 50,000 babies born from CARE treatments, which is amazing. With RI Witness, we were very attracted to gathering data across clinics. Our labs are very standardized, and we all follow the same protocols. Clinical practices might be slightly different, but when you get down to the lab, we operate the same. So, the data captured across the thirteen clinics will be really useful for us.
RI Witness and quality digitalization is a great step into improving the entire patient fertility journey. All clinics will have the knowledge to improve lab performance and that is an opportunity that makes sense for us.
Dr. Tucker: We have already seen growing confidence in each of the labs, which in itself is a significant benefit. RI Witness system is many tools in one – an objective tool that can give clinics an amplified level of transparency and risk management tool with electronically verified transcripts. When we can inspect performance outcomes, current and prospectively, we can create the opportunity to share best SOPs to improve industry standards and lead the way in integrity and transparency towards patients.